The efficacy of compression therapy in addressing the majority of varicose and lymphatic diseases cannot be overemphasized enough. However, the applicability of these formulations is not restricted to this context only but is much more advanced in Wound care, specifically for pain management. Today, we will review in depth the mechanism of compression, its effects on the healing of complicated wounds, and its benefits for patients.
Understanding Compression Therapy
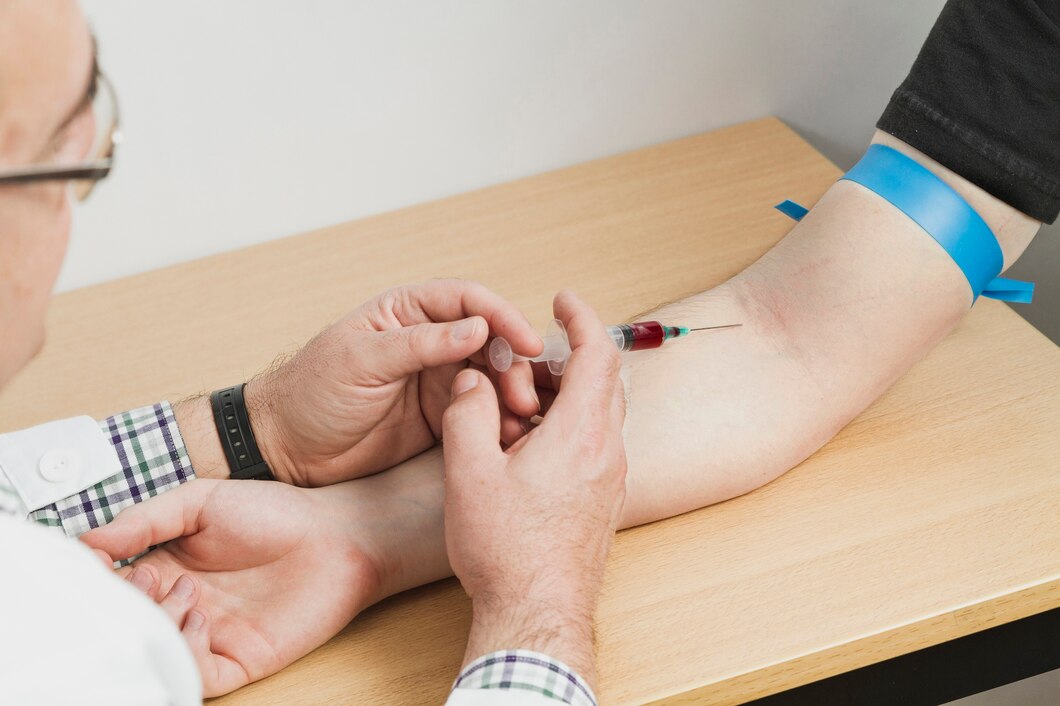
Compression therapy, therefore, refers to how bandages, garments, or special devices are used to apply pressure to a certain limb or the wound area. This method employs particular force utilizing various techniques focused on troubles with the venous and lymphatic systems with edema by inflicting less tissue damage.
In the broad spectrum of wound care, compression plays an important role in disorders that involve venous ulcers, Lymphedema, and diabetic foot ulcers, where there is compromised blood supply and oxygenation of tissues, which slows down the healing process.
Mechanisms of Action
The effectiveness of compression therapies in wound healing outcomes is associated with multifactorial aspects. Reduced venous hypertension is central to the compression function exerted by the VF on the superficial veins, which thus facilitates blood circulation to the heart.
Increased blood circulation helps to reduce swelling and bring nutrients and oxygen for repair to cells where they are needed. It also decreases swelling, low oxygen in injured tissues, and scar tissue formation to heal the injured portion of the skin with new epidermal cells.
Efficacy in Venous Ulcer Management
Venous ulcers are a global challenge for both patients and providers, entailing a lengthy recovery process that is quite exhausting for both parties. Compression therapy is essential in the treatment of venous ulcers because it addresses the root cause of venous insufficiency and enhances wound healing.
Regardless, several investigations demonstrated that compression therapy favors faster ulcer healing, a decrease in the ulcer’s recurrence, and the affected patient’s quality of life enhancement. Compression therapy enhances venous circulation and prevents chronic edema, infection, and necrosis, thus enhancing the care for venous ulcer patients.
Role in Lymphedema Management
Lymphedema is a disease that manifests as swelling of the tissues due to the accumulation of fluid within the lymphatic system that cannot be drained efficiently. Currently, it is only managed through compression therapy that involves the use of outside mechanical pressure to facilitate the action of the lymph pump and decrease volume in the limbs.
They palliate symptoms, delay the disease progression, decrease cellulitis risks, and enhance lymphatic configuration by capturing and preventing fluid accumulation with compression garments/ bandages. In combination with other techniques such as MLD, exercise, and others, compression therapy is an indispensable component of management approaches for Lymphedema.
Impact on Diabetic Foot Ulcers
Diabetic foot ulcers, one of the most common and deadly diabetes complications, can cause amputation and extreme pain. Peripheral neuropathy and vascular impairment cause diabetic foot ulcers and their failure to heal, highlighting the need for wound treatment.
When paired with offloading devices and wound debridement, compression is a successful treatment. It helps cure ulcers, reduce infections, and prevent amputations. By optimizing tissue blood flow, minimizing edema, and improving the wound environment, compression therapy enhances other treatments for DM and foot ulcers.